Introduction:
Pelvic pain can be a complex and multifaceted challenge for both patients and healthcare providers. For one 29-year-old woman, a persistent history of pelvic discomfort, burning during urination, and pain radiating to the lower abdomen with deeper penetration
marked the beginning of a long diagnostic odyssey. Her story underscores the importance of thinking outside the box, reassessing assumptions, and pushing for answers when initial treatments fail.
The Beginning of the Journey:
It all started 18 months ago when she began experiencing pelvic pain and pressure, coupled with burning sensations while urinating. Over time, the pain extended to her lower abdomen, becoming particularly intense during deeper penetration. Concerned, she sought medical attention. A battery of tests, including urinary tract and pelvic evaluations, yielded no answers. Her symptoms persisted, leaving her and her healthcare providers frustrated.
When Standard Approaches Fall Short:
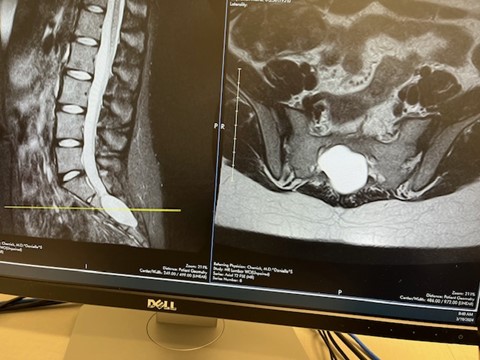
Given the unusual presentation and lack of response to initial treatments, her case was referred to a physiatrist specializing in complex pain syndromes. The physiatrist’s thorough evaluation included advanced imaging, which uncovered an unexpected finding: a massive intrasacral meningeal cyst and multiple Tarlov’s cysts at several spinal levels. These fluid-filled sacs, though often asymptomatic, had in her case become a significant source of her pain and discomfort.

The Road to Surgery:
The discovery of the cysts prompted consultations with two specialists in spinal surgery and neurology. After careful consideration, surgery was recommended. Four months ago, she underwent a complex procedure that not only addressed the identified cysts but
also revealed additional complications, including erosion of her sacrum. This required reconstruction of the sacral lamina, a critical step in stabilizing her spine and alleviating her symptoms.
Recovery and Reflection:
Post-surgery, her recovery is ongoing but promising. Her story is a poignant reminder that persistent pain should never be dismissed, even when initial tests suggest no obvious cause. The erosion of her sacrum and the unexpected findings during surgery highlight the need for vigilance and comprehensive investigation in challenging cases.
Key Takeaways:
- Listen to the Patient: Persistent symptoms, even in the absence of clear diagnostic findings, merit continued investigation.
- Think Outside the Box: Complex cases often require multidisciplinary approaches and the willingness to explore less common diagnoses.
- Reassess Regularly: If treatments are not yielding results, revisiting the diagnosis and considering alternative explanations can be life-changing.
- Advocate for Yourself: For patients, persistence and self-advocacy are essential. Trust your body and push for answers if something doesn’t feel right.
Conclusion: This young woman’s journey from unexplained pelvic pain to a rare spinal diagnosis and successful surgery illustrates the power of persistence and collaboration in healthcare. Her story serves as an inspiring reminder to healthcare providers to remain curious and to patients to never stop seeking solutions.